Disclaimer: This post/article/blog is for informational purposes only and is not a substitute for professional mental health advice, diagnosis, or treatment. Always seek the advice of qualified health providers with any questions you may have regarding mental health concerns.
Infographics were created by a mix of professionals and people with ADHD and selected by Katie to reflect what she has experienced personally and professionally.
Table of Contents
- The Nature of Clinical Depression
- The Impact on Daily Functioning
- The Role of Brain Chemistry
- The Temporary Nature of Depression
- Understanding Depression Through a Disability Lens
- Treatment and Recovery
- The Impact on Loved Ones
- The Fear Factor
- Adjusting Expectations
- The Role of Compassion
- The Importance of Professional Help
- The Intersection of Depression, Trauma History, ADHD, and ASD
- Resources for More Information
In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.

Hi, I'm Katie.
I’m a neurodivergent mental health counselor. I specialize in helping neurodivergent adults navigate complex intersectional identities and comorbid mental health, trauma, or substance use.
This blog is shaped by my own education and experiences as a therapist. It's not a definitive resource, not a textbook to be quoted or a manual to be followed. Instead, it's an offering—by someone with an unusual mix of perspectives and skills. Someone who has spent too long living in and witnessing the growing disconnect between people and the cost of harmful misunderstandings.
Introduction

Depression is often misunderstood. Many view it as simply feeling sad or unmotivated, which can be overcome with positive thinking or willpower. However, clinical depression is far more than that – it's a serious medical condition that can profoundly impact every aspect of a person's life.
In this blog post, we'll explore clinical depression and examine how it changes the rules and expectations for daily life and affects those around the person experiencing it. We will also explore how it interacts with Trauma, ADHD, and Autism.
The Nature of Clinical Depression
Clinical depression, also known as major depressive disorder, is a complex mental health condition that affects millions of people worldwide. It's characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities once enjoyed. For some people, they experience anger and frustration instead of sadness. But it's much more than just feeling down – it's a condition that can significantly impair a person's ability to function in daily life.
The two most common types of depression:
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
Depression can affect anyone regardless of age, gender, race or ethnicity, income, culture, or education. Research suggests that genetic, biological, environmental, and psychological factors play a role in the disorder.
When clinical depression settles in, it's as if the person is no longer fully themselves. Their thoughts, behaviors, and physical capabilities can be dramatically altered. This change is not a choice or a weakness – it results from changes in brain chemistry and function.
For some people, depression may be a short-term condition that doesn't significantly impair their ability to work or engage in daily activities. For others, it can be a long-term, severely debilitating condition that meets the criteria for disability status.
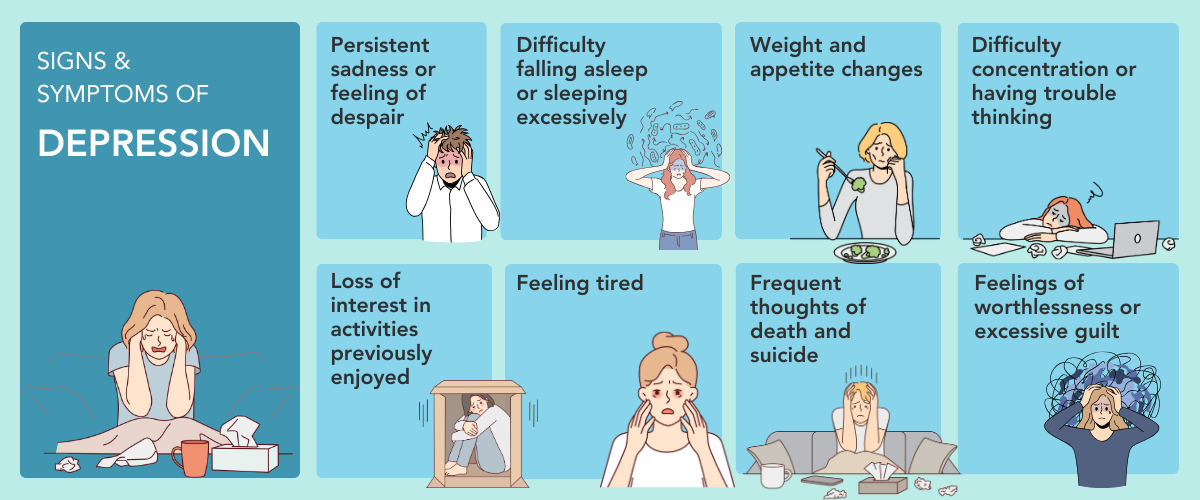
Common signs and symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet responsibilities or ignoring other important roles
- Problems with sexual desire and performance
Symptom lists from National Institute of Mental Health - Depression
The Impact on Daily Functioning
Let's break down how clinical depression can affect various areas of daily life:
- Personal Care and Hygiene: Depression can make self-care feel impossible. The energy required to shower, brush teeth, or change clothes can be overwhelming. This isn't laziness – it's a symptom of the condition.
- Nutrition and Eating Habits : Depression often affects appetite, leading to either significant weight loss or gain. Preparing meals can feel impossible, leading to reliance on unhealthy convenience foods or skipping meals entirely.
- Home Maintenance: Keeping a living space clean and organized requires energy and motivation – both of which are in short supply during depression. Dishes may pile up, laundry may go unwashed, and general clutter may accumulate.
- Work or School Performance: Concentration, memory, and decision-making are all impaired by depression. This can lead to decreased productivity, missed deadlines, and potential job loss or academic struggles.
- Social Interactions: Depression often leads to social withdrawal. Maintaining relationships requires energy that a depressed person may not have, leading to isolation and loneliness.
- Physical Health: The fatigue associated with depression can lead to a sedentary lifestyle, which, combined with potential changes in eating habits, can negatively impact physical health.
The Role of Brain Chemistry
Clinical depression is fundamentally a biological condition. While life events, stress, and other external factors can trigger or exacerbate depression, the underlying mechanism involves changes in brain chemistry and function.
Key neurotransmitters involved in depression include:
- Serotonin: Often called the "feel-good" chemical, low levels are associated with depression
- Norepinephrine: Plays a role in alertness and energy levels
- Dopamine: Involved in motivation and pleasure
When these chemical messengers are out of balance, it can lead to the symptoms we recognize as depression. This is why medication can be a crucial part of treatment for many people with clinical depression. Antidepressants work by altering the levels and interactions of these neurotransmitters, helping to restore balance and alleviate symptoms.
The Temporary Nature of Depression
It's crucial to emphasize that while clinical depression is a serious condition, it is often temporary (compared to lifelong developmental conditions like ADHD or Autism). With proper treatment and support, many people can recover and return to their previous level of functioning. However, the duration can vary significantly – from weeks to months to years.
Understanding depression as a temporary condition is essential for several reasons:
- It offers hope to those experiencing depression
- It encourages seeking treatment, as there is a possibility of improvement
- It helps supporters maintain patience and empathy during the recovery process
Sometimes, depression is very hard to treat and requires more than standard therapy and medications. See the resource article at the end of this post if you want to read more about “treatment-resistant depression.”
Understanding Depression through a Disability Lens
Like physical disabilities, depression can limit a person's ability to perform everyday tasks, engage in work or social activities, and maintain relationships. However, because it's invisible, it's often misunderstood or dismissed.
When someone is clinically depressed, the rules and expectations of daily life change dramatically. Once simple tasks can become monumental challenges.
For a person in the depths of depression:
- Getting out of bed can feel like climbing a mountain
- Taking a shower might require as much energy as running a marathon
- Preparing a meal can seem as complex as solving a complicated mathematical equation
- Engaging in social interaction might feel as daunting as public speaking to a crowd of thousands
In this context, a day on which a person manages to get up, take a shower, feed their pets, and take out the trash can be considered a significant success. This shift in what constitutes achievement is crucial to understanding that depression may be a disability for some.
Whether depression qualifies as a disability for an individual depends on several factors:
- Severity: The intensity of symptoms and their impact on daily functioning.
- Duration: How long the depressive episode has lasted or is expected to last.
- Impact on Work: The extent to which depression affects one's ability to perform job duties.
- Treatment Response: How the individual responds to treatment and management strategies.
Whether or not an individual pursues official disability status, understanding depression through a disability lens can help advocate for needed support and accommodations.
It's crucial to remember that the decision to seek disability status is highly individual and should be made in consultation with healthcare providers and, if necessary, legal professionals.
Treatment and Recovery
While clinical depression is a serious condition, it is treatable. The most effective approach often involves a combination of:
- Medication: Antidepressants can help correct the chemical imbalances in the brain
- Psychotherapy: Techniques like cognitive-behavioral therapy can help change negative thought patterns and develop coping strategies
- Lifestyle changes: Regular exercise, a healthy diet, and good sleep habits can support recovery
- Social support: Connecting with others, even in small ways, can be beneficial
It's important to note that recovery is often a gradual process. Minor improvements, like having the energy to do laundry or cook a meal, should be celebrated as significant steps forward.
The Impact on Loved Ones
Clinical depression doesn't just affect the individual experiencing it – it also impacts those around them. Family members, friends, and colleagues often notice something isn't right, even if they can't pinpoint exactly what's wrong. This can lead to a range of reactions:
- Confusion: Not understanding why their loved one has changed
- Frustration: Particularly if they view the symptoms as a choice or lack of effort
- Helplessness: Wanting to help but not knowing how
- Fear: Worrying about their loved one's wellbeing and future
It's important to emphasize that the person with depression is not choosing to be this way, and it's not their fault. The changes in behavior and mood are symptoms of their condition, not a reflection of their feelings towards their loved ones.
The Fear Factor
Fear is a common reaction among those close to someone with clinical depression. This fear can stem from various sources:
- Fear for the person's safety, especially if they express suicidal thoughts
- Fear of saying or doing the wrong thing and making the situation worse
- Fear of the unknown – not knowing how long the depression will last or if the person will fully recover
- Fear of loss – of the relationship, of the person they once knew
Addressing these fears through education about depression and open communication can help both the person with depression and their support network navigate this challenging time.
Adjusting Expectations
For both the person with depression and their support network, adjusting expectations is crucial. This might mean:
- Setting smaller, achievable goals for daily tasks
- Recognizing that recovery isn't linear – there will be good days and bad days
- Understanding that "getting back to normal" might take time
- Celebrating small victories as significant achievements
The Role of Compassion
Compassion – self-compassion and compassion from others – plays a vital role in navigating clinical depression. For the person experiencing depression, self-compassion means:
- Recognizing that depression is not a personal failure
- Allowing oneself to rest without guilt
- Acknowledging small accomplishments
- Seeking help without shame
For those supporting someone with depression, compassion involves:
- Offering support without judgment
- Being patient with the recovery process
- Educating themselves about depression
- Taking care of their own mental health
The Importance of Professional Help
While support from loved ones is invaluable, professional help is often necessary for managing clinical depression. Mental health professionals can:
- Provide an accurate diagnosis
- Develop a tailored treatment plan
- Monitor progress and adjust treatment as needed
- Offer strategies for managing symptoms
- Provide a safe space to express feelings and concerns
Encouraging someone with depression to seek professional help, or even offering to help them find a therapist or make an appointment, can be a crucial step in their recovery journey.
The Intersection of Depression, Trauma History, ADHD, and ASD
It's crucial to recognize that depression often co-occurs with other conditions and experiences, particularly trauma, Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD). Understanding these intersections can provide a more comprehensive view of an individual's experience and inform more effective treatment approaches.
Trauma History and Depression: A history of trauma, whether from childhood experiences or adult events, can significantly increase the risk of developing depression. The relationship between trauma history and depression is complex and multifaceted:
- Neurobiological Impact: Trauma can alter brain structure and function in ways similar to depression, affecting areas responsible for emotion regulation, memory, and stress response.
- Cognitive Patterns: Traumatic experiences can lead to negative beliefs about oneself, others, and the world, which are also common in depression.
- Emotional Regulation: Trauma survivors may struggle with emotional regulation, increasing vulnerability to depressive episodes.
- Avoidance and Numbing: Depression can sometimes serve as a coping mechanism to numb overwhelming emotions related to past trauma.
- Triggers and Flashbacks: For those with trauma history, specific triggers can lead to re-experiencing traumatic memories, potentially precipitating or exacerbating depressive episodes.
- Interpersonal Difficulties: Past trauma can affect one's ability to form and maintain relationships, potentially leading to isolation and depression.
For individuals with both a trauma history and depression, treatment often needs to address both conditions simultaneously. Trauma-informed care, therapies like EMDR (Eye Movement Desensitization and Reprocessing), and body-based approaches may be beneficial alongside traditional depression treatments.
ADHD and Depression: ADHD and depression frequently co-occur, and each can exacerbate the symptoms of the other:
- Chronic Stress: The ongoing challenges of managing ADHD symptoms can contribute to the development of depression.
- Executive Function: Both conditions affect executive functioning, compounding challenges in daily life, such as organization, time management, and task completion.
- Self-Esteem: Repeated difficulties due to ADHD can lead to low self-esteem, a common feature in depression.
- Motivation: Depression can worsen ADHD symptoms like inattention and motivation difficulties.
- Emotional Dysregulation: Both conditions can involve difficulty regulating emotions, leading to mood swings and interpersonal challenges.
Treatment for individuals with both ADHD and depression often involves a combination of medication management, cognitive-behavioral strategies, and skills training to address the unique challenges posed by both conditions.
ASD and Depression: Individuals on the autism spectrum are at higher risk for developing depression, often due to:
- Social Challenges: Social interaction and communication difficulties can lead to isolation and loneliness.
- Sensory Sensitivities: Chronic stress from navigating a world that can be overwhelming on a sensory level.
- Masking: The exhaustion from trying to "fit in" or mask autistic traits can contribute to depression.
- Executive Function: Planning, organization, and adaptability challenges can lead to chronic stress and feelings of inadequacy.
- Special Interests: Depression can interfere with the enjoyment of special interests, a crucial source of happiness for many autistic individuals.
For autistic individuals with depression, treatment may need to be adapted to account for differences in communication style, sensory needs, and cognitive processing.
The Compounding Effect: When depression co-occurs with trauma history, ADHD, or ASD, the impact on daily functioning can be even more profound. For example:
- An individual with ADHD and a trauma history might struggle not only with focus and organization but also with intrusive memories and hypervigilance, all of which can be exacerbated by depression.
- An autistic person with depression and a history of trauma might find social interactions even more challenging as they navigate sensory sensitivities, social communication differences, depressive symptoms, and trauma-related anxiety.
- Someone with ADHD, depression, and a trauma history might find that both depressive symptoms and trauma-related avoidance compound their difficulty with motivation.
Tailored Treatment Approaches: Recognizing these intersections highlights the importance of individualized, comprehensive treatment plans. A one-size-fits-all approach to depression treatment may not be effective for individuals also dealing with trauma history, ADHD, or ASD. Instead, treatment should address each person's unique constellation of symptoms and challenges.
This might involve:
- Trauma-Informed Care: Understanding how past experiences impact current symptoms and behaviors.
- Sensory-Friendly Practices: Essential for autistic individuals or those with sensory processing differences.
- Executive Function Support: Providing strategies to manage the combined challenges of depression and ADHD on organization and task completion.
- Medication Management: Careful consideration of how medications might interact when treating multiple conditions.
- Holistic Approaches: Incorporating body-based therapies, mindfulness practices, or creative arts therapies that can address trauma, neurodivergence, and depression simultaneously.
- Psychoeducation: Helping individuals and their support systems understand the complex interplay between trauma, neurodevelopmental differences, and depression.
- Strength-Based Approaches: Recognizing and building upon the unique strengths that often accompany neurodivergence, even in the context of depression and trauma.
By understanding and addressing these intersections, we can provide more effective support and treatment for individuals navigating the complex landscape of depression alongside trauma history and neurodevelopmental conditions. This comprehensive approach addresses immediate symptoms and fosters long-term resilience and well-being.
Conclusion and Resources for more information
Clinical depression is a complex, challenging condition that can temporarily but seriously remove a person's ability to function in daily life. It changes the rules of a successful day, turning simple tasks into monumental achievements. It affects the individual and those around them, often instilling fear and confusion in loved ones.
Remember, while clinical depression is a severe condition, it is often temporary. With the proper support, treatment, and understanding, recovery is possible. Every small step – from taking a shower to feeding pets to taking out the trash – is a victory worth celebrating on the path to healing.
By fostering compassion, adjusting expectations, and promoting understanding, we can create a more supportive environment for those grappling with clinical depression, helping them navigate this temporary disability and move toward recovery.
For more information
- National Institute of Mental Health - Depression
- Mayo Clinic article on Treatment-Resistant Depression
- Substance Abuse and Mental Health Services Administration
We welcome all people, regardless of race, ethnicity, age, religion, gender identity, sexual identity, relationship status, body composition, or disability. We pledge to provide a safe space for our team and our clients.
Recent Posts