Disclaimer: This post/article/blog is for informational purposes only and is not a substitute for professional mental health advice, diagnosis, or treatment. Always seek the advice of qualified health providers with any questions you may have regarding mental health concerns.
Infographics were created by a mix of professionals and people with ADHD and selected by Katie to reflect what she has experienced personally and professionally.
Table of Contents
Seeking Engagement: How Neurological Understimulation and ADHD Can Look Like Depression
- Introduction
- Understanding ADHD and Its Neurological Basis
- Neurological Basis of ADHD
- The Concept of Understimulation in ADHD
- Understimulation and an Interest-Based Nervous System
- How Understimulation Manifests in Daily Life
- Similarities Between Understimulation and Depression
- Differentiating ADHD Understimulation From Clinical Depression
- Strategies for Managing Understimulation
- When to Seek Professional Help
- Conclusion and Key Takeaways

Hi, I'm Katie.
I’m a neurodivergent mental health counselor. I specialize in helping neurodivergent adults navigate complex intersectional identities and comorbid mental health, trauma, or substance use.
This blog is shaped by my own education and experiences as a therapist. It's not a definitive resource, not a textbook to be quoted or a manual to be followed. Instead, it's an offering—by someone with an unusual mix of perspectives and skills. Someone who has spent too long living in and witnessing the growing disconnect between people and the cost of harmful misunderstandings.
Introduction

Attention Deficit Hyperactivity Disorder (ADHD) is a complex neurodevelopmental condition that affects millions of people worldwide. While most are familiar with its hallmark symptoms of inattention, hyperactivity, and impulsivity, there's a lesser-known aspect of ADHD that can significantly impact an individual's life: neurological understimulation.
Neurological understimulation can manifest in ways that look like depression to friends, family, medical providers, therapists, and the person themselves. This misinterpretation can contribute to misdiagnosis, ineffective treatment strategies, decades of suffering and underemployment, and the development of conditions like substance abuse and trauma.
In this exploration, we'll delve into the intricate relationship between ADHD, neurological understimulation, and depressive symptoms. By understanding this connection, we can shed light on the experiences of many individuals with ADHD and pave the way for more accurate understanding and interventions.
Understanding ADHD and Its Neurological Basis
ADHD is characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.
In psychology, "interfering with functioning or development" refers to how a condition like ADHD impacts an individual's ability to perform daily tasks, meet age-appropriate expectations, or progress through typical developmental stages between birth and adulthood.
- "Interfering with functioning" includes
-
- Impairment in the ability to complete tasks at work or school
- Hindering the management of daily responsibilities
- Affecting social interactions and relationships
- Impacting the ability to follow through on commitments
- Disrupting organization and time management skills
- “Interfering with development” includes
-
- Delaying or altering the acquisition of age-appropriate skills
- Affecting cognitive development, mainly executive functions
- Influencing emotional development and self-regulation
- Impacting social skill development and peer relationships
- Possibility of academic or professional underachievement relative to the individual's potential
These interferences are significant enough to cause noticeable problems in multiple areas of life, distinguishing ADHD from typical variations in behavior or temporary difficulties. The impact on functioning and development often persists over time and across different settings, such as home, school, and work.
ADHD is also associated with differences in brain structure, function, and neurotransmitter activity, particularly in the dopamine and norepinephrine systems. (See blog post on ADHD 101)
These neurological differences contribute to the core symptoms of ADHD and set the stage for understanding neurological understimulation.
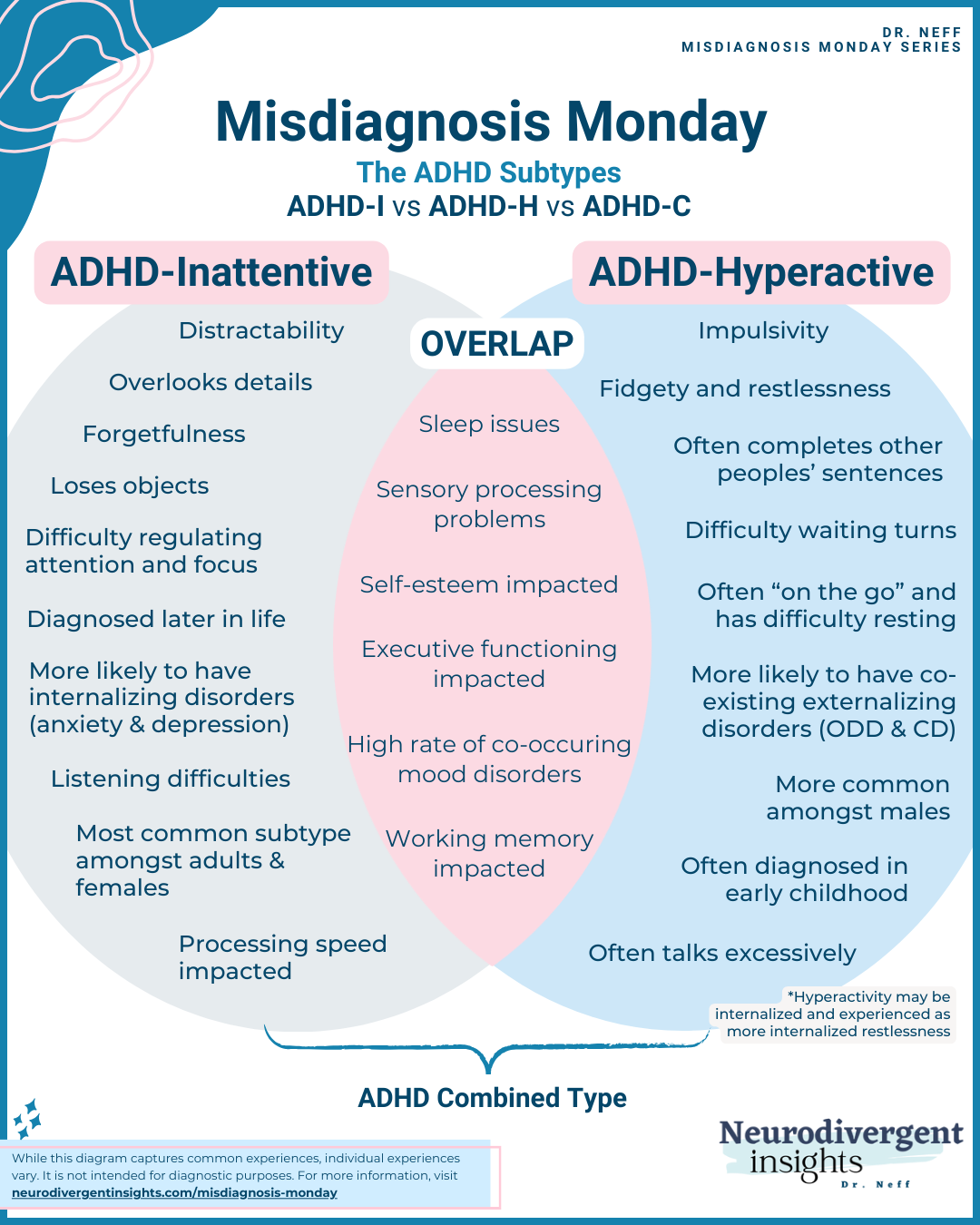
The three primary symptom categories of ADHD are:
- Inattention: Difficulty focusing, easily distracted, trouble following instructions, apparent forgetfulness.
- Hyperactivity: Excessive movement, fidgeting, inability to sit still, constant feelings of restlessness.
- Impulsivity: Acting without thinking, interrupting others, making rash decisions, and having difficulty with delayed gratification.
These symptoms can manifest differently across individuals and may change over time. It's important to note that ADHD is not simply a behavioral disorder but has deep neurological roots.
Neurological Basis of ADHD
To understand neurological understimulation in ADHD, we must first explore the condition's underlying brain mechanisms.
ADHD is associated with differences in brain structure, function, and neurotransmitter activity:
- Brain structure: Individuals with ADHD often show slight differences in the size and activity of specific brain regions, particularly those involved in attention, impulse control, and executive function.
- Neurotransmitter imbalances: ADHD is linked to irregularities in dopamine and norepinephrine systems. These neurotransmitters play crucial roles in attention, motivation, and reward processing.
- Executive function deficits: ADHD affects executive functions, which are higher-order cognitive processes that help us plan, organize, and regulate our behavior and emotions.
These neurological differences contribute to the core symptoms of ADHD and set the stage for understanding neurological understimulation.
The Concept of Understimulation in ADHD
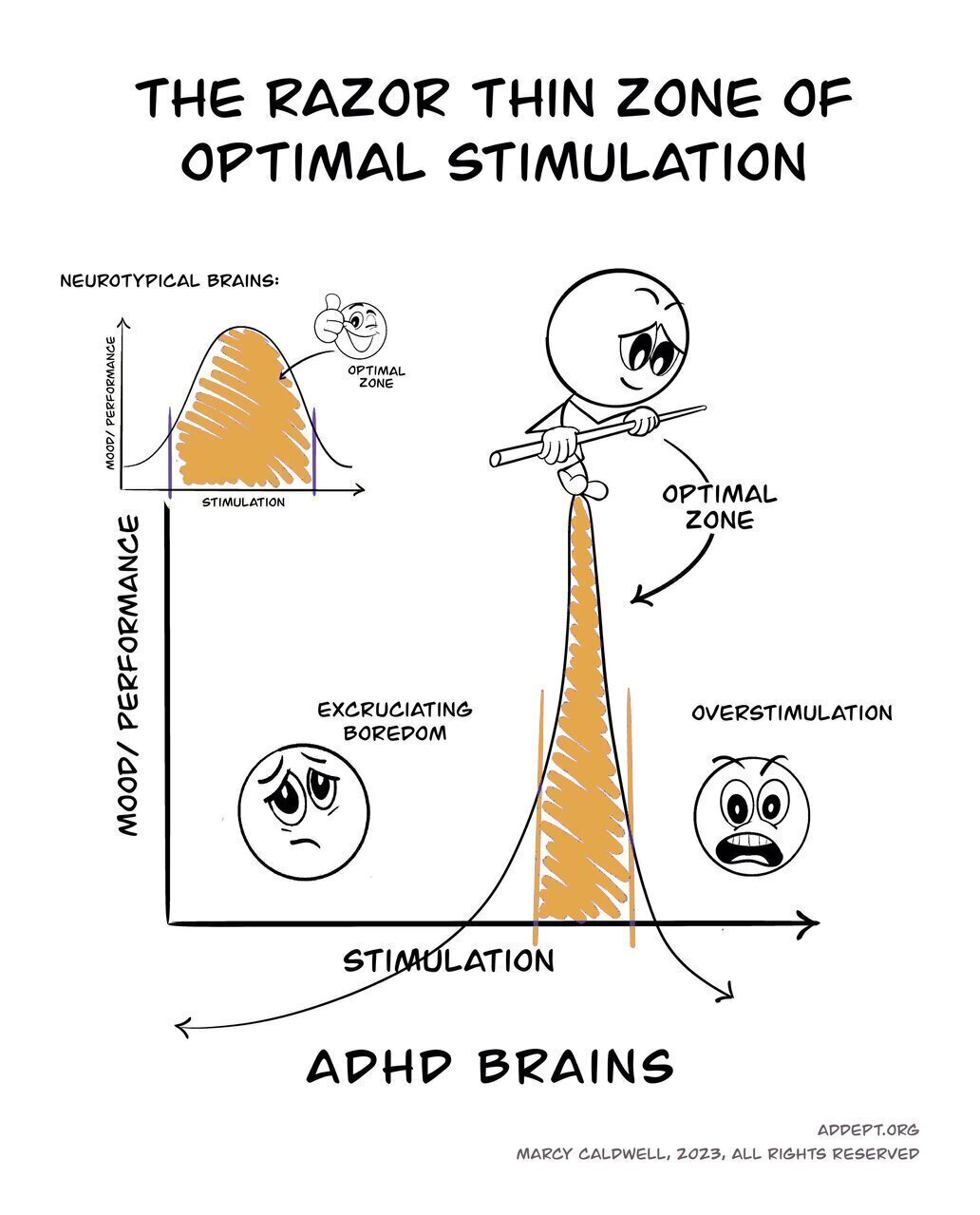
Neurological understimulation in ADHD refers to a state where the brain doesn't receive enough stimulation to maintain optimal arousal and engagement. This concept is closely tied to the "optimal stimulation theory" proposed by researchers studying ADHD.
The ADHD brain often has lower baseline levels of dopamine, a neurotransmitter associated with motivation, pleasure, and attention. To compensate for this understimulation, individuals with ADHD may unconsciously seek more stimulating activities or environments.
Key points about understimulation in ADHD:
- Dopamine deficit: The ADHD brain often has lower baseline levels of dopamine, a neurotransmitter associated with motivation, pleasure, and attention.
- Seeking stimulation: To compensate for this understimulation, individuals with ADHD may unconsciously seek more stimulating activities or environments.
- Difficulty with mundane tasks: Routine or less stimulating tasks can be particularly challenging, as they fail to provide the necessary neurological activation.
- Fluctuating attention: Attention may spike for highly stimulating activities but wane quickly for less engaging tasks.
Understanding this concept proves crucial, as it may help explain many behaviors and experiences common in ADHD that the core symptom categories don't fully capture.

Understimulation and an Interest-Based Nervous System
The concept of neurological understimulation in ADHD is closely tied to what Dr. William Dodson, a psychiatrist specializing in ADHD, calls the "interest-based nervous system." This framework helps explain why individuals with ADHD often struggle with chronic understimulation and why traditional motivational approaches (such as rewards, incentives, punishments, and "natural" consequences) may be less effective for individuals with ADHD compared to those without the condition.
Importance-Based Nervous System (Typical in people without ADHD):
- In this system, neurons release dopamine when an individual expects to receive a reward or achieve something deemed important.
- This dopamine release influences attention, motivation, and movement, effectively engaging the person in tasks that are considered significant or have future benefits.
- As a result, neurotypical individuals are less likely to experience chronic understimulation, as they can maintain engagement through the anticipation of future rewards or consequences.
Interest-Based Nervous System (ADHD):
In contrast, the ADHD brain releases dopamine only when it perceives specific criteria:
- Passion (and Play)
- Interest
- Novelty or Newness
- Competition, Challenge or Cooperation
- Hurry or Urgency
This selective dopamine release explains why individuals with ADHD often experience understimulation in everyday situations that don't meet these criteria.
When the ADHD brain encounters a task or situation that meets one of these criteria it releases dopamine at levels comparable to a neurotypical brain, temporarily alleviating the state of understimulation and allowing the person to engage with less difficulty.
The interest-based nervous system in ADHD creates a predisposition to understimulation. Tasks or environments that don't provide novelty, interest, challenge, or urgency fail to trigger sufficient dopamine release, leading to a state of neurological understimulation. This understimulation can manifest as inattention, restlessness, or even symptoms that resemble depression.
How Understimulation Manifests in Daily Life
Neurological understimulation can significantly impact various aspects of an individual's life:
- Work and academic performance: Difficulty engaging with less stimulating tasks can lead to procrastination, incomplete work, or underachievement.
- Relationships: Seeking stimulation may manifest as interrupting conversations, frequently changing topics, or appearing disinterested in slower-paced interactions.
- Hobbies and interests: Intense focus on highly stimulating activities and rapid loss of interest in others.
- Emotional regulation: Understimulation can lead to irritability, restlessness, or a pervasive sense of boredom.
- Sleep patterns: Difficulty "shutting off" the mind, leading to delayed sleep onset or irregular sleep schedules.
- Risk-taking behaviors: Some individuals may engage in risky activities to increase stimulation.
These manifestations of understimulation can profoundly affect an individual's quality of life and overall well-being. Notably, many of these experiences can closely resemble symptoms of depression.
Similarities Between Understimulation and Depression
The effects of neurological understimulation in ADHD can often mirror symptoms of clinical depression, leading to potential confusion in diagnosis. Here are some key areas where these conditions may appear similar:
- Low motivation: Both understimulated individuals with ADHD and those with depression may struggle to initiate or complete tasks, even ones they typically enjoy.
- Fatigue: Chronic understimulation can lead to mental exhaustion, similar to the persistent fatigue experienced in depression.
- Anhedonia: The inability to feel pleasure from activities once enjoyed is a hallmark of depression but can also occur in ADHD when usual activities fail to provide adequate stimulation.
- Social withdrawal: Both conditions can result in reduced social interaction for different reasons.
- Sleep disturbances: Irregular sleep patterns are common in both ADHD and depression.
- Difficulty concentrating: While a core symptom of ADHD, concentration problems are also prevalent in depression.
- Emotional dysregulation: Mood swings, irritability, and emotional outbursts can occur in both conditions.
- Negative self-perception: Chronic understimulation in ADHD can lead to feelings of inadequacy and low self-esteem, similar to the negative self-view often seen in depression.
These overlapping experiences can make it challenging for individuals and even healthcare professionals to distinguish between ADHD-related understimulation and clinical depression.
Differentiating ADHD Understimulation From Clinical Depression
For information about Depression in general, See the post on Depression 101.
While there are similarities, several key factors can help differentiate between ADHD understimulation and clinical depression:
- Situational variability: Individuals with ADHD often experience rapid mood changes based on the level of stimulation in their environment. In contrast, depressive symptoms tend to be more persistent across different situations.
- Response to stimulation: Those with ADHD typically show improved mood and functioning when engaged in stimulating activities, while individuals with depression may not experience such immediate improvements.
- Underlying thought patterns: Depression often involves persistent negative thoughts about oneself, the world, and the future. In ADHD, negative thoughts are usually more directly related to frustration with symptoms or specific situations.
- History and onset: ADHD symptoms, including understimulation, are usually present from childhood and remain relatively consistent over time. Depression often has a more distinct onset and may be tied to specific life events or stressors.
- Physical symptoms: While both conditions can affect sleep and energy levels, depression is more likely to cause significant changes in appetite and psychomotor function.
- Cognitive patterns: Individuals with ADHD often report racing thoughts or mental restlessness, whereas depression is more commonly associated with slowed thinking and rumination.
- Motivation for change: Those with ADHD typically want to engage and do things but struggle with initiation. In depression, there's often a more pervasive lack of desire to engage in activities.
- Reward sensitivity: People with ADHD often maintain sensitivity to immediate rewards, while those with depression may experience a global reduction in reward responsiveness.
It's crucial to note that these distinctions are not always clear-cut, and ADHD and depression can co-occur. A thorough clinical assessment is necessary for accurate diagnosis and appropriate treatment planning.
Strategies for Managing Understimulation
For individuals with ADHD experiencing understimulation, several strategies can help increase engagement and improve overall functioning:
- Environmental modifications: Create a stimulating work or living environment with appropriate lighting, background noise, and visual interest.
- Task structuring: Break larger tasks into smaller, more manageable steps and intersperse routine activities with more engaging ones.
- Time management techniques: Use tools like the Pomodoro Technique to create focused work periods alternating with short breaks.
- Physical activity: Regular exercise can help increase dopamine levels and improve overall brain function.
- Mindfulness and meditation: These practices can help increase awareness of understimulation and improve focus.
- Cognitive Behavioral Therapy (CBT): Education can help develop coping strategies and reframe negative thought patterns.
- Stimulating hobbies: Engage in activities that provide appropriate mental or physical stimulation.
- Medication: For some individuals, ADHD medications can help regulate neurotransmitter levels and reduce understimulation.
- Sleep hygiene: Establish consistent sleep patterns to support overall brain health and function.
- Nutrition: A balanced diet with adequate protein, complex carbohydrates, and omega-3 fatty acids can support brain health.
Individuals can personalize strategies based on individual needs and preferences. It's often helpful to work with a healthcare professional or ADHD coach to develop an effective management plan.
When to Seek Professional Help
While self-management strategies can be effective, there are times when professional help is necessary. Consider seeking assistance from a mental health professional if:
- Symptoms significantly impact daily functioning: If understimulation or other ADHD symptoms severely affect work, school, or relationships.
- Self-management strategies aren't sufficient: If the techniques mentioned earlier aren't providing adequate relief.
- Mood symptoms worsen or persist: If feelings of sadness, hopelessness, or lack of motivation become severe or long-lasting.
- Co-occurring conditions are suspected: If you think you might be experiencing both ADHD and depression or other mental health conditions.
- Considering medication: A psychiatrist can assess whether medication might be beneficial and guide its use.
- Need for personalized strategies: A therapist or ADHD coach can help develop tailored coping mechanisms.
- Difficulty differentiating symptoms: If you're unsure whether your experiences stem from ADHD, depression, or another condition.
- Thoughts of self-harm: If you're experiencing any thoughts of harming yourself, seek immediate professional help.
Remember, seeking help is a sign of strength, not weakness. Mental health professionals can provide valuable insights, support, and treatment options.
Conclusion
The intersection of ADHD, neurological understimulation, and depressive symptoms represents a complex but essential area of mental health. By understanding how understimulation in ADHD can mimic depression, we can better address the unique challenges faced by individuals with ADHD and provide more targeted support.
Key takeaways
- Neurological understimulation is a common but often overlooked aspect of ADHD.
- Understimulation can manifest in ways that closely resemble depression, potentially leading to misdiagnosis.
- While there are similarities, ADHD understimulation and clinical depression have distinct characteristics.
- Various strategies can help manage understimulation, from environmental modifications to cognitive techniques.
- Professional help is crucial for accurate diagnosis and comprehensive treatment planning.
As our understanding of ADHD continues to evolve, it's crucial to consider the full spectrum of experiences associated with the condition. By recognizing the role of neurological understimulation, we can develop more nuanced approaches to diagnosis and treatment, ultimately improving outcomes for individuals with ADHD.
For those navigating the challenges of ADHD, remember that your experiences are valid. Whether you're dealing with classic ADHD symptoms, under-stimulation, or co-occurring depression, support and effective treatments are available. Don't hesitate to contact mental health professionals who can provide the guidance and care you deserve.
By fostering greater awareness and understanding of these complex neurological processes, we can work towards a future where individuals with ADHD receive more accurate diagnoses, targeted treatments, and compassionate support. This knowledge not only benefits those with ADHD but also contributes to a more nuanced and inclusive understanding of neurodiversity in our society.
We welcome all people, regardless of race, ethnicity, age, religion, gender identity, sexual identity, relationship status, body composition, or disability. We pledge to provide a safe space for our team and our clients.
Recent Posts